 08 Mar 2020
08 Mar 2020
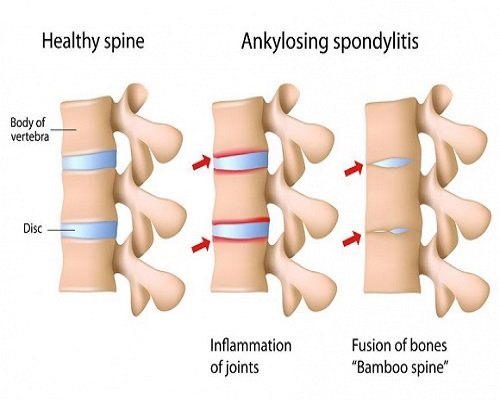
Ankylosing spondylitis is an inflammatory disease that causes some of the bones to fuse which then affects the spines flexibility and also the body posture of the patient. It is mostly observed that men are more prone to it than women. The symptoms of the disease can be observed from adulthood.
It mostly affects:
1. Lower Back
2. The base of the Spine and Pelvis
3. Vertebrates in the lower back
4. Joints in Spine
5. Heels
6. Pelvis
7. The cartilage between the breastbone and ribs
8. In severe cases formation of new bone
In severe cases, a new bone is formed in this new bone bridges the gap between vertebrae and eventually fuses sections of vertebrae. Which later become stiff and inflexible. In some cases it stiffens your rib cage, restricting your lung capacity and function.
Causes:
There is no specific cause, but it’s said genetic factors may also affect it. People having a gene called HLA-B27 are at a greater risk of developing ankylosing spondylitis. But not every individual having it may suffer from it. It is observed more in men as compared to women specifically during adulthood.
One such case study is about Ankylosing Spondylitis in a young patient. During the initial examination, Dr. Pravin Patil a rheumatologist in Pimpri Chinchwad diagnosed symptoms of Ankylosing Spondylitis in a very young patient. He then came up with a remedial plan of action considering the patient’s age and condition. It was then observed that the patient was responding excellently to biologics injections. In such cases, Patients can walk without support and lead a fairly normal life post-treatment. Biological injections should be considered as a treatment option in patients who are not doing well on conventional medications. Biological injections are prescribed by Rheumatologists who have experience in using this relatively new therapy. In this case, the patient has visibly gained a lot post-treatment by Dr. Pravin Patil. Who is known for his impeccable contribution in the field of Rheumatology & Ankylosing Spondylitis. He is one of the best rheumatologist in pimpri chinchwad.
 15 Jan 2018
15 Jan 2018
RA factor is a protein (antibody) that is measurable in the blood with a routine blood test. A positive RA factor test means that level of rheumatoid factor in patient’s blood is high. A positive RA factor test is mainly used as a supportive tool in making the diagnosis of rheumatoid arthritis.
Our immune system produces healthy proteins (antibodies) that fight off infections caused by bacteria and viruses. Sometimes, bad antibodies are produced by the immune system which can attack healthy tissue. RA factor is a bad antibody protein produced by patient’s immune system.
It is unknown what triggers our immune system to produce rheumatoid factor. It is thought to be a combination of genetics and other external risk factors.
RA factor test is used by doctors to help in diagnosing rheumatoid arthritis. Approximately 70% of rheumatoid arthritis patients test positive for RA factor.
A negative RA factor test does not rule out the diagnosis of rheumatoid arthritis. In fact, there is no single test to diagnose rheumatoid arthritis. The diagnosis is made from a combination physical symptoms and medical history supported by various blood tests such as RA factor, anti-CCP antibodies and elevated inflammatory markers. Newer tests like anti-CCP antibodies are much more specific for rheumatoid arthritis.
Patients who test negative for RA factor but have signs and symptoms may still be diagnosed with rheumatoid arthritis. This is seen in around 30% patients with rheumatoid arthritis (seronegative).
Rheumatoid arthritis affects different patients in different ways. Rheumatoid arthritis patients with a positive RA factor test have the potential for a more aggressive disease course. Keep in mind this isn’t always the case. If RA factor is tested and symptoms are detected early, a diagnosis can be quickly reached. Treatment should be started as soon as possible to joint damage.
The level of RA factor can fluctuate during the course of the disease but it does not correlate with disease activity and it does not normalise with treatment. If you have rheumatoid arthritis, it is not necessary to monitor the level RA factor. Inflammatory markers such as ESR and CRP are often elevated during active disease and can be good markers to monitor treatment response.
For more information please visit amolg9.sg-host.com
